 March 2025 Issue
March 2025 Issue
Clinical Nutrition: HCAHPS Patient Satisfaction Survey Revisions
By Wendy Phillips, MS, RD, LD, FAND, FASPEN, and Grant Randall, JD
Today’s Dietitian
Vol. 27 No. 3 P. 8
Recommended Strategies for Hospital Food and Nutrition Departments
Hospitals measure patient satisfaction and perception of the care received in order to continuously focus on process improvement while also meeting regulatory requirements imposed by CMS.1 In use since 2006 by mandate from CMS, the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) measures patients’ experiences of hospital care through standardized survey questions sent after a patient has been discharged from the hospital. The results are publicly reported on the Hospital Compare website,2 which helps people compare the quality of care across hospitals to make informed decisions on where to receive care.
The HCAHPS survey doesn’t include questions that specifically measure patient satisfaction related to food service, nor does it collect information about some of the other services provided within the hospital.3 Therefore, hospitals often pay for additional patient satisfaction surveys, such as Press Ganey or NRC Health. This allows them to assess those services to determine improvement strategies since many of these services influence whether patients will decide to receive care at that hospital in the future. These supplemental surveys usually include food service-related questions, although there is no standardization of questions from one survey tool to the next.
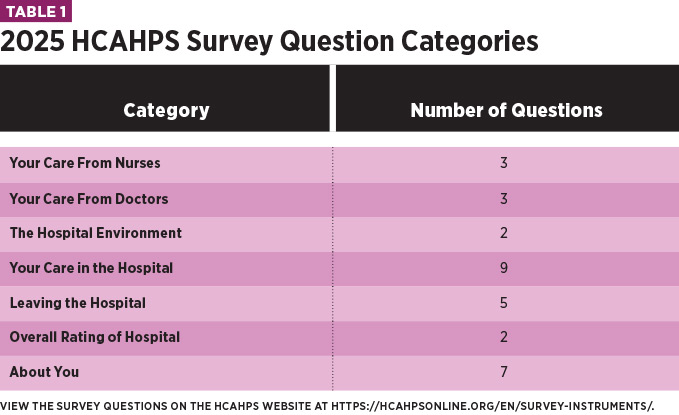
Similarly, HCAHPS doesn’t ask questions related to the clinical care provided by RDs or nutrition and dietetic technicians, registered (NDTRs).3 However, many questions ask about the care provided by “doctors, nurses, and other hospital staff,” and patients may consider interactions with RDs and NDTRs when responding to those questions. Therefore, the clinical nutrition team should become familiar with the questions and provide services in a manner that would drive positive responses. See Table 1 for more information.
Changes to HCAHPS Survey
CMS periodically updates the survey to reflect changes in the health care environment and patient expectations.1 Several significant changes have gone into effect as recently as January 1, 2025.4 Impactful elements of the CMS update will focus on survey modes, care coordination, restfulness, and symptom measurement and information. The changes align with CMS’s ongoing efforts to reduce burden on consumers and providers, increase health care efficiency, and promote person-centered care.1 The survey is meant to provide hospitals with meaningful feedback and actionable items to improve care and support innovation.
Changes in survey logistics are included in the 2025 updates.4 Optional web-first modes will be offered in addition to mail and phone. Patient-Mix Adjustments will be updated to accommodate this change. To offset the increased number of HCAHPS questions and encourage a higher response rate, CMS will now limit the number of supplemental survey questions, such as those used by Press Ganey or NRC Health, to 12. Patients will also now have 49 days from discharge to answer the survey instead of the previous 42 days. In addition, CMS is removing the prohibition of proxy respondents, so patients may designate someone to complete the survey on their behalf. Survey vendors will be required to administer a Spanish version of the survey to all Spanish language-preferring patients.4
High-level details of the changes to the questions are as follows3:
• Within the demographics “About You” section, the number of languages spoken at home will be simplified for respondents to choose “English, Spanish, Chinese, or another language.”
• Emergency department admission questions will be completely changed to distinguish between planned and unplanned stays.
• New HCAHPS submeasure questions for care coordination, restfulness of hospital environment, and information about symptoms will be added, as well as revisions to the responsiveness of hospital staff and “About You” questions. Questions pertaining to care transition will be removed. These changes will increase the current 29 survey items to 32.
Table 1 provides an overview of the 2025 survey with a URL to the survey tool itself with specific questions.
Recommended Strategies
Hospitals still have the option to choose question(s) that assess food services within the 12 supplemental questions, but may or may not choose to do so, depending on other priorities. Food and nutrition departments should start as soon as possible to work with hospital administrators to determine their strategy for 2025 and beyond. Without defined food- and nutrition-specific questions, it’ll become much more difficult to track departmental performance and patients’ perceptions of the food services.
As vice president of patient experience for Compass One Healthcare, a company that supports almost one thousand hospitals to define excellence in food and nutrition services, Dusty Deringer, PhD, provides recommended strategies to assist hospitals in navigating possible changes to supplemental survey questions given the new 12-question limit. “Since current and future practices related to food and nutrition survey questions aren’t standardized from one hospital or health system to the next, we provide different recommendations for consideration”6 (see Table 2).
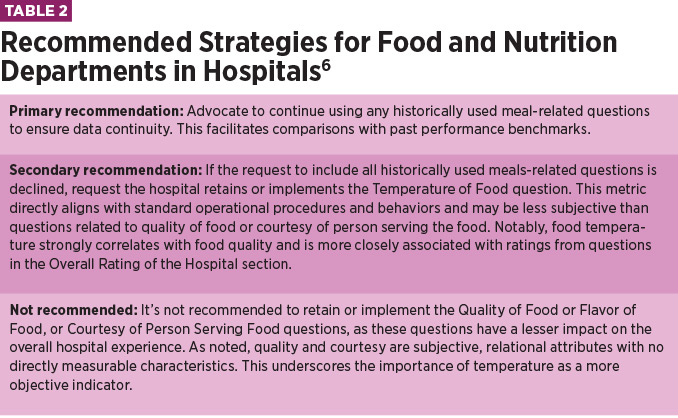
It may be possible to request the inclusion of food-related questions as part of the 12 supplemental questions, even if none were included historically. If that scenario exists, Deringer recommends a question related to food temperature for the reasons noted above.
It’s vital to discuss the issue of benchmark comparison groups with hospital administration, regardless of which recommendation is followed. Many hospitals will choose to use fewer or zero food service-related questions, which will significantly alter the comparison groups used for percentile rankings. Furthermore, we have seen major care systems that have gone away from a food service-related question but quickly return to the question upon realizing that they had lost an efficient and unbiased means of tracking performance for such a critically used department.
Final Thoughts
A patient’s perception of their care experience is a vital component of healing, as it can influence patient safety, outcomes, and adherence to treatment plans.7 Hospitals with higher publicly reported patient satisfaction results will be able to attract new patients and retain existing ones. Hospital food and nutrition departments can gain valuable insights for continuous process improvement through patient satisfaction surveys. RDs, NDTRs, and food service leaders should have proactive conversations with hospital administrators in regard to the upcoming CMS requirements for the HCAHPS survey process.
— Wendy Phillips, MS, RD, LD, FAND, FASPEN, is a regional vice president for Morrison Healthcare, providing leadership and operational oversight for hospital food and nutrition programs. She has been an RD for over 20 years, previously serving as an adult and neonatal nutrition support clinician and in clinical nutrition director positions.
— Grant Randall, JD, is the national director of consumer experience for Compass One Healthcare. He and his teams work with clinical and operational support staff in hundreds of facilities to elevate all aspects of the user experience. His passion is developing emotional intelligence in caregivers and effecting cultural change through staff engagement.
References
1. HCAHPS: patients' perspectives of care survey. Centers for Medicare and Medicaid Services website. https://www.cms.gov/medicare/quality/initiatives/hospital-quality-initiative/hcahps-patients-perspectives-care-survey. Updated September 6, 2023. Accessed September 3, 2024.
2. Hospital Compare website. https://hospitalcompare.io/. Accessed September 3, 2024.
3. CAHPS hospital survey. Hospital Consumer Assessment of Healthcare Providers and Systems website. https://hcahpsonline.org/en/survey-instruments/. Updated May 10, 2024. Accessed September 3, 2024.
4. Centers for Medicare and Medicaid Services. Code of federal regulations: Medicare and Medicaid programs and the children’s health insurance program; hospital inpatient prospective payment systems for acute care hospitals and the long-term care hospital prospective payment system and policy changes and fiscal year 2025 rates; quality programs requirements; and other policy changes, 42 CFR Parts 405, 412, 413, 431, 482, 485, 495, and 512. https://public-inspection.federalregister.gov/2024-17021.pdf. Updated August 28, 2024. Accessed September 3, 2024.
5. The HCAHPS survey – frequently asked questions. Centers for Medicare and Medicaid Services website. https://www.cms.gov/medicare/quality-initiatives-patient-assessment-instruments/hospitalqualityinits/downloads/hospitalhcahpsfactsheet201007.pdf. Accessed September 3, 2024.
6. Morrison Healthcare. Adjusting meals-related patient satisfaction questions [Press Release]. Published June 5, 2024.
7. Burgener AM. Enhancing communication to improve patient safety and to increase patient satisfaction. Health Care Manag (Frederick). 2020;39(3):128-132.
