Today’s Dietitian
Vol. 26 No. 6 P. 32
Take this course and earn 2 CEUs on our Continuing Education Learning Library
Dysphagia, or difficulty swallowing, affects 8% of the world’s population and an estimated 15 million Americans.1,2 While individuals of all ages experience dysphagia, it mostly affects infants and older adults, and prevalence increases with age.2 Nearly 65% of individuals experience dysphagia after a stroke, making it the leading cause of dysphagia, followed by neurological diseases and cancers of the head and neck, respectively.2,3
Because swallowing ability directly impacts the ability to consume sufficient energy and nutrients, dysphagia is a known risk factor for dehydration and malnutrition.4 Studies show nearly 40% of individuals with dysphagia are at risk of malnutrition, and the odds of having malnutrition are double in long term care residents with dysphagia.5,6
Diet modifications are often necessary to prevent foods and fluids from entering the airway, also known as aspiration, which can lead to pneumonia, respiratory infection, and even death.7 While the speech language pathologist (SLP) is responsible for determining the appropriate diet modification, RDs are uniquely qualified to ensure the nutritional adequacy of modified diets and to prevent and treat malnutrition.8
In 2013, the International Dysphagia Diet Standardisation Initiative (IDDSI) was created to address the need for common terms and definitions to describe texture-modified foods and thickened liquids around the world.9 In January 2017, the Academy of Nutrition and Dietetics (the Academy) and the American Speech-Language-Hearing Association (ASHA) announced their support of IDDSI, and in October 2021, IDDSI replaced the National Dysphagia Diet (NDD) as the only texture-modified diet recognized by the Academy’s Nutrition Care Manual.10 Though not mandatory, IDDSI implementation is underway in facilities around the world thanks to the efforts of RDs, SLPs, food service directors, and other partners.11
This continuing education course will review the role of RDs in dysphagia management and explore the new evidence-based standard for defining texture-modified foods and thickened liquids.
Swallowing Physiology
Understanding normal swallow function can help RDs recognize when a problem exists and warrants further investigation by an SLP or other discipline. Because food and air share the same entrance—the pharynx—swallowing requires careful coordination between cranial nerves and muscles of the oral cavity, pharynx, larynx, and esophagus to prevent aspiration.12
Swallowing is divided into three phases: oral, pharyngeal, and esophageal. During the oral phase, food is voluntarily chewed and moistened with saliva to form a bolus. The tongue then propels the bolus to the back of the pharynx. During the pharyngeal phase, the soft palate, larynx, and epiglottis work together to ensure the bolus passes into the esophagus rather than the trachea, the main airway into the lungs. During the esophageal phase, the bolus passes down the esophagus into the stomach via peristalsis.12
A disruption to any of these phases can lead to dysphagia. For example, brain damage from stroke, cerebral palsy, Parkinson’s disease, and other nervous system disorders interferes with nerves responsible for initiating and controlling the swallow. Disorders like muscular dystrophy and myasthenia gravis, a chronic autoimmune disease, that weaken muscles all over the body can also weaken those involved in swallowing.
Causes of Dysphagia
In infants and children, dysphagia may present due to structural abnormalities like cleft lip and palate; developmental delays; prematurity and low birth weight; neurological disorders like cerebral palsy, traumatic brain injury, and botulism; sensory processing disorders; and other medical conditions including gastroesophageal reflux disease and heart and lung diseases.13
Although taste, smell, and saliva production decline with age and swallowing muscles naturally weaken due to a general decline in muscle mass, dysphagia is not inevitable with aging.14 Rather, dysphagia is a consequence of age-related diseases including neuromuscular and neurodegenerative disorders like stroke, dementia, multiple sclerosis, and amyotrophic lateral sclerosis (also known as Lou Gehrig’s disease); cancers of the mouth, throat, and esophagus and their treatments; and others including esophageal stricture, gastroesophageal reflux disease, HIV, spinal cord injury, lung inflammation, and endotracheal intubation.1,14
Clinical Manifestations
Many signs and symptoms associated with dysphagia can be observed at mealtimes. These include choking, coughing, gagging, drooling, frequent throat clearing, repeated swallowing, pocketing of food in the mouth, leaking of liquids from the mouth, and slow eating.15 Individuals may report pain with swallowing (odynophagia), difficulty chewing or moving the tongue, a feeling of food getting stuck in the throat or chest, inability to finish meals due to fatigue, and avoidance of specific food textures. RDs should also be cognizant of unintentional weight loss and signs of dehydration from inadequate food or fluid intake. In some cases, individuals may accidentally inhale food and fluids without showing any signs or symptoms, a condition known as silent aspiration.
Screening for Dysphagia
Screening methods include bedside swallowing evaluations, mealtime observations, interviews with patients or caregivers, and water swallow tests.16 Although dysphagia screening protocols will vary by facility, the World Gastroenterology Organisation recommends “urgent” screening in any patient with ongoing weight loss and recurring chest infections.2 Considering 42% to 67% of people present with dysphagia within three days of a stroke, the World Gastroenterology Organisation also recommends screening stroke patients within 24 hours after the stroke and before oral intake.2
Role of the RD in Dysphagia Screening
Like all members of the interdisciplinary care team, RDs are critical in the early identification of individuals who require a more comprehensive swallowing assessment.16 Reviewing the medical record for diagnoses commonly associated with dysphagia is an important first step. These include dementia, head and neck cancers, brain tumors, stroke, and traumatic brain or head injury.17 Dysphagia seen in cancers of the head, neck, and throat may be caused by an obstructive tumor, surgical removal or reconstruction of structures involved in swallowing, or side effects of chemotherapy and radiation, like esophageal strictures, mucositis, dry mouth, and fibrosis. Following endotracheal intubation, up to 93% of patients will experience dysphagia due to muscle atrophy, delirium, and inflammation of the throat.18
The Eating Assessment Tool (EAT-10) is a validated and widely used tool in clinical and community settings around the world.19,20 The EAT-10 can be completed by patients or providers and contains 10 questions about the severity of an individual’s symptoms, including weight loss, pain, and effort when swallowing. When mealtime observation is possible, RDs should look for warning signs including choking, coughing, pocketing of food, avoidance of food textures, drooling, and the presence of a wet and gurgled voice after eating. During interviews, rather than asking if someone has trouble swallowing, it is best to ask specific questions such as, “Do you cough, choke, or gag when you try to swallow?”, “Does it feel like food is getting stuck in your throat when you swallow?”, or “How much effort does swallowing typically require?” The EAT-10 questionnaire can be a useful guide as it includes questions about weight loss, social behaviors, stress, pain, and pleasure when eating.
The nutrition-focused physical exam can also provide information about physical factors that impact swallowing ability, though RDs should receive the proper training from an SLP prior to incorporating these physical findings into their assessment.15,17 For example, RDs can assess tongue strength and range of motion, swallow and cough reflex, oral hygiene including dentition, cognitive impairments, and muscle loss.17 The nutrition-focused physical exam can also be used to evaluate weight changes, signs of dehydration and nutrient deficiencies, and functional status.
Diagnosis and Treatment
Although dysphagia can be diagnosed at the bedside, objective swallow exams are indicated if more information is needed and if silent aspiration is suspected.15 The two most common exams are the videofluoroscopy swallow study, also known as the modified barium swallow, and the flexible endoscopic evaluation of swallowing. SLPs typically perform these exams in collaboration with radiologists, otolaryngologists, or other physicians. A single exam is unlikely to capture the full picture so other tests like CT scans, esophageal manometry, and upper endoscopy may be performed.14
Treatment approaches aim to provide adequate nutrition and improve swallow safety. These include muscle-strengthening exercises that alter swallowing physiology or compensatory strategies that improve swallow safety such as posture changes, chin tucks, head turns, and diet modifications. Modifying the texture of foods and the thickness of liquids is a common practice to reduce the risk of aspiration. As an example, the SLP may prescribe a pureed diet for someone who has poor tongue control and cannot bite or chew food or recommend adding thickener to drinks if someone cannot manage the fast flow of water, milk, or other thin liquids.9 Although the use of thickened liquids has been associated with adverse effects on health and quality of life, it remains a common strategy to prevent aspiration.21,22
If within the goals of care, nutrition support via enteral or parenteral nutrition may be recommended for individuals who are unable to meet their nutritional needs by mouth, or if eating and drinking are considered unsafe.
Nutritional Implications of Dysphagia
Inadequate food and fluid intake is a major consequence of dysphagia that can lead to unintended weight loss, dehydration, and malnutrition. Nearly 40% of all individuals with dysphagia are at risk of malnutrition, and malnutrition has been reported in up to 50% of individuals with dysphagia residing in long term care facilities.4,5 In older adults, the loss of skeletal muscle that naturally occurs with aging known as sarcopenia contributes to a decline in swallow function and increases the risk of malnutrition. The term sarcopenic dysphagia refers to difficulty swallowing caused by sarcopenia.23 This is a particular concern since older adults are already at risk of nutrient deficiencies due to normal physiological changes.24
Decreased intake among people with dysphagia is multifactorial. It may be a consequence of pain, increased time and effort required to eat, avoidance of certain foods, cognitive impairments, and decreased self-feeding ability.4,23 Other factors include less enjoyment when eating, embarrassment, depression, and anxiety.4,25
Research points to the use of texture-modified diets as another driver of inadequate energy, fluid, and nutrient intake in this population. Taste and unappealing food aesthetics are common barriers to acceptance of modified diets and improved mealtime satisfaction.26 A 2020 systematic review of 35 studies across 12 countries found that individuals on modified diets (n=2,245) had lower energy and fluid intake when compared with regular diets.26 In this study, pureed diets were more likely to be deficient in fiber, potassium, calcium, zinc, magnesium, vitamin D, and vitamin E, which is often attributed to the added water needed to blend these foods into the correct consistency.
Another study found that 75% of long term care residents with oropharyngeal dysphagia (n=28) were dehydrated while on thickened liquids.27 Reduced fluid intake while on thickened liquids has been attributed to poor taste, lack of flavor and thirst-quenching ability, increased satiety due to their viscosity and the fiber content of thickeners, and reduced quality of life.27 It is critical that RDs assess fluid intake given that dehydration increases the risk of kidney dysfunction, impaired mental status, constipation, and infection.23,27
Nutrition Management of Dysphagia
In addition to food and liquid modification, nutrition-related interventions for dysphagia include the use of fortified foods, oral nutritional supplements (ONS), vitamin and mineral supplementation, feeding assistance or accommodation, nutrition education and counseling, environmental modifications, and if necessary, nutrition support.17,26
Fortified Foods
Fortified foods have extra calories, protein, and/or fat added and are appropriate for individuals who are losing weight or have trouble meeting their nutrient needs.17 For example, facilities could puree meals with milk, cream, or broth instead of water, or use whole milk fortified with milk powders when making grits, oats, or soups. A 2020 systematic review found improved nutrient intake when fortifying foods with vitamin powder, rapeseed oil, infant cereal, and whey protein.26 In this study, the most effective intervention for improving nutrition and mealtime satisfaction on pureed diets was shaping or molding pureed foods to resemble regular foods using three-dimensional molds, which improved protein intake by 32% to 36%.26
ONS
ONS can also be used to help clients meet their nutritional needs. Studies have shown the use of ONS improves energy, protein, nutrient intake, and quality of life in malnourished populations and those with dysphagia.28,29 A 2022 cross-sectional study published in the journal Nutrients examined dietary intake and nutritional status among aged care residents (n=85) receiving texture-modified diets with and without ONS, 38% of which were malnourished and 48% were at risk of malnutrition. Residents received ONS two to five times per day, with three times per day being the most common frequency. Those who received ONS consumed an average of 1,554 kcal/day and 63 g of protein/day, compared with 1,155 kcal/day and 46 g of protein/day in those not receiving ONS. Ninety-three percent of residents on ONS met their daily protein needs, compared with 46% without ONS.30
Regular ONS may be too thin for some individuals, and it can be difficult to achieve the correct consistency when trying to manually thicken them. Several food companies now offer prethickened ONS, which have been shown to improve compliance and nutrient and fluid intake when compared with manually thickened ONS.31,32
Other strategies to optimize food and fluid intake include offering snacks between meals, minimizing distractions when eating, and providing adaptive eating devices or meal set-up assistance.17 When acceptance of the modified food or fluid texture is limited, RDs can try to offer foods that are naturally at the prescribed texture. For example, hummus, applesauce, or smooth yogurt without fruit pieces on a pureed diet. Initial and ongoing education on the importance of adequate nutrition and the rationale for diet modification can encourage oral intake as well.17
The NDD
In July 1997, members of the American Dietetic Association (now the Academy) met with SLPs, food scientists, and food manufacturers to discuss the need for standardized terminology to classify dysphagia diets across facilities in the United States.33 Frustration was mounting as the lack of consistent, objective, and reliable terms caused confusion and safety concerns when a patient transitioned from one place to the next, and it cost time and money for facilities to clarify diet orders and reevaluate patients.23,33
The task force called their initiative the NDD, which was published by the American Dietetic Association in 2002. The NDD classified foods into four levels: Level 1 (Dysphagia-Pureed), Level 2 (Dysphagia-Ground or Mechanically Altered), Level 3 (Dysphagia-Advanced), and Level 4 (Regular). Liquids were classified based on their viscosity, or resistance to flow: thin, nectarlike, honeylike, and puddinglike.34
Facilities continued to vary in their diet terminology, definitions, and testing methods. Ambiguous terms like “soft” and “chopped” were difficult to interpret, and there was no guarantee that one facility defined their modified diets in the same way as the next.35 Citing a lack of scientific research to support NDD, ASHA never fully supported the initiative.36
There remained no standardized language on a global scale.23,35 A 2017 systematic review that included a survey of dysphagia diets in 33 countries found 27 different names used to describe five levels of liquid thickness, and 54 different names for five levels of food textures.1 In the United States and Canada, the four terms used to classify liquids from least to most modified are thin, nectar, honey, and pudding. But in Asia, terms like honey, nectar, and pudding are not understood and facilities use the following five terms (in order of increasing thickness): thin, slightly thick, mildly thick, medium thick, and extra thick.1 This lack of global diet terminology has been a major barrier to understanding the benefits of diet modification throughout the world and improving dysphagia outcomes. For instance, because the consistency of nectar-thick liquids varies around the world, demonstrated benefits of nectar-thick liquids in one country may not apply to other parts of the world.1
The Transition to IDDSI
In 2013, a group of experts from 10 countries met to discuss the need for a global standard to describe texture-modified foods and drinks. The group represented the fields of nutrition and dietetics, speech pathology, occupational therapy, gastroenterology, nursing, food science, mechanical engineering, and physiotherapy. The goal was to create a framework that would apply to all care settings and to people of all ages and cultures and would provide specific definitions and objective testing methods. The proposed benefits of the framework included improvements in patient safety and communication among health care professionals and advancements in research related to dysphagia treatment outcomes.1
In 2017, after three years of work, the committee published the IDDSI framework along with standardized food testing methods. To date, IDDSI has been implemented in over 30 countries and translated into 22 different languages with 12 more in progress.37 While IDDSI is not mandatory, both the Academy and ASHA recognize IDDSI as their new standard of practice and the Academy marked May 1, 2019, as the official launch date for its implementation in the United States. In October 2021, the Academy announced that IDDSI would be the only texture-modified diet recognized by the Nutrition Care Manual.10
The IDDSI Framework
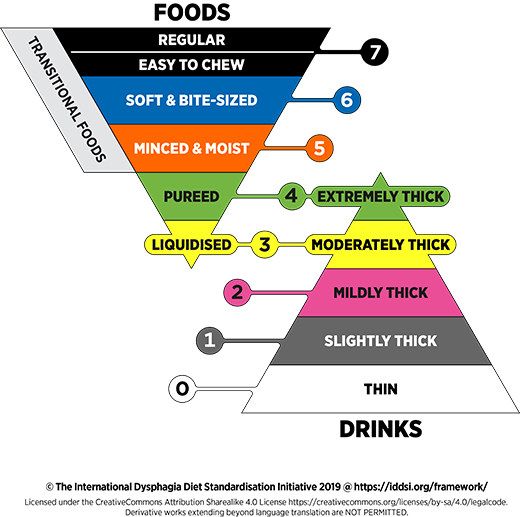
As image 1 illustrates, the IDDSI framework comprises eight levels of modified foods and liquids, each with its own name, color, and number.9 The food levels from most to least modified are Level 3 (Liquidized), Level 4 (Pureed), Level 5 (Minced & Moist), Level 6 (Soft & Bite-Sized), and Level 7 (Regular and Easy to Chew). The liquid levels from most to least modified are Level 4 (Extremely Thick), Level 3 (Moderately Thick), Level 2 (Mildly Thick), Level 1 (Slightly Thick), and Level 0 (Thin). Food levels 3 (Liquidized) and 4 (Pureed) overlap with liquid levels 3 (Moderately Thick) and 4 (Extremely Thick) because they have similar flow and texture characteristics.9
Level 7 is unique in that it contains two textures. Level 7 (Regular) is a regular diet with no restrictions to size or textures and is therefore suitable for individuals who do not have chewing or swallowing problems. Level 7 (Easy to Chew) is suitable for individuals who do not have swallowing problems but do require foods to be soft and tender because of weak chewing muscles.9
Levels 5 through 7 are classified as transitional foods because they start at one texture and change to another with moisture or a change in temperature. For example, ice cream that melts in the mouth, or cheese puffs that break down with the addition of saliva.9
IDDSI Testing Methods
The purpose of IDDSI’s testing methods is to ensure foods and drinks have the correct texture and thickness. They were designed to be convenient, inexpensive, and accessible, requiring only a fork, spoon, syringe (for drinks), and visual observation. Acknowledging that forks are not used in some parts of the world, IDDSI provides instructions for testing with fingers or chopsticks when indicated. Audit sheets are available on the IDDSI website to help facilities determine whether their foods and drinks meet the intended criteria.38
Thickened drinks (Levels 0 to 3) and liquidized foods (Level 3) are evaluated using the IDDSI Flow Test. Liquids are classified based on how much liquid remains in a 10 mL syringe after flowing for 10 seconds. For example, drinks (or liquidized foods) are classified as IDDSI Level 0 (Thin) if less than 1 mL of liquid remains in the syringe.39
Because extremely thick liquids (Level 4) will not flow through a syringe, the Fork Drip Test or Spoon Tilt Test is used. During the Fork Drip Test, thickness is determined based on how well a sample holds its shape on a fork and how much of the sample flows through its prongs. The Fork Drip Test is also used to confirm the consistency of foods at Levels 3 to 5 (Liquidized, Pureed, and Minced & Moist).39
The Spoon Tilt Test ensures foods are cohesive and not too sticky and is used for IDDSI Level 4 (Pureed/Extremely Thick) and Level 5 (Minced & Moist). To pass this test, the food should hold its shape on a spoon and fall off easily with minimal residue remaining. An example of a food that would not pass the Spoon Tilt Test is peanut butter, which is firm and sticky and leaves a significant amount of residue when flicked off the spoon.39
The Fork Pressure Test and Spoon Pressure Test determine how hard a food is and is used to assess foods at Level 4 (Pureed) to Level 7 (Easy to Chew). During these tests, foods are classified based on their behavior after pressure is applied with a fork or spoon. For example, foods at Level 5 (Minced & Moist) should mash easily and the nail should not turn white when pressure is applied. Level 6 (Soft & Bite-Sized) foods should be cut, squashed, or broken apart easily with pressure from a fork or spoon, which may turn the nail white.39
Transitional foods are tested by applying 1 mL of water to a thumb-size sample and waiting one minute before applying pressure with a fork until the nail turns white. To pass the test, the sample should break apart easily and not return to its original shape.39
The complete IDDSI Framework, including detailed definitions, testing instructions for each diet level, and answers to frequently asked questions
can be found on the IDDSI website.9
Comparing NDD and IDDSI
Compared with NDD, IDDSI provides more objective descriptions along with simple testing methods for each food and drink level. IDDSI also expands the levels of liquid consistencies. Whereas NDD classifies thickened liquids from least to most modified as nectarlike, honeylike, and puddinglike (or spoon-thick), IDDSI replaces these with mildly thick, moderately thick, and extremely thick. The new framework includes an additional level called slightly thick (Level 1), which falls between thin and mildly thick.40
NDD Level 1 (Dysphagia-Pureed) shares the same name and texture as IDDSI Level 4 (Pureed), but IDDSI provides more objective descriptions and testing methods. NDD Level 2 (Dysphagia-Mechanically Altered) is similar to IDDSI Level 5 (Minced & Moist), but IDDSI outlines requirements for the size of minced food (4 mm X 15 mm or less for adults, or 2 mm X 8 mm or less for pediatric) and added moisture from thickened sauce or gravy to minimize the risk of choking.9,40
NDD Level 3 (Dysphagia-Advanced) is similar to IDDSI Level 6 (Soft & Bite-Sized), but IDDSI takes the diameter of the airway into consideration and restricts food piece sizes to no longer than 15 mm (8 mm for pediatric). NDD Level 3, also referred to as “Regular Soft,” may also align with IDDSI Level 7 (Easy to Chew).40
The RD’s Role in IDDSI Implementation
Along with food service directors and SLPs, RDs are leading IDDSI implementation around the world by raising awareness of the need for standardized language, forming multidisciplinary task forces, and creating implementation calendars. RDs can review their institution’s current diet labels, descriptions, and testing methods and align them with the IDDSI framework, a process called “mapping.” RDs can also consider dual/transitional labeling in their notes and communication, like writing “moderately thick per the IDDSI framework” in parenthesis when referring to honey-thick liquid recommendations.41 These and other suggestions are available in the implementation guide that IDDSI has created specifically for clinicians.41
Putting It Into Practice
Dysphagia affects people of all ages, but older adults are at greater risk of developing dysphagia due to age-related disease and a decline in swallow function. RDs play an invaluable role in the interdisciplinary management of dysphagia, from screening those at risk to managing weight loss, malnutrition, and dehydration.
Collaboration between RDs and SLPs can optimize an individual’s food and fluid intake. While the SLP is responsible for diagnosing and treating the swallowing disorder and determining the safest diet texture, RDs are responsible for ensuring the diet is nutritionally adequate and determining the need for dietary restrictions or diet liberalization.17,42 Both integrate the individual’s personal preferences and cultural foodways into their recommendations.42
In 2019, IDDSI replaced NDD as the new standard for defining dysphagia diets, and implementation is already happening around the world. RDs can begin the process at their facility by raising awareness of IDDSI, forming implementation teams, reviewing their institution’s own diet labels and descriptions, and dual labeling in their clinical communications. The Academy has established IDDSI as the new standard of practice for RDs, and although implementation is not mandatory, the Academy encourages all providers to adopt the new framework to ensure patient safety.
— Emily Guzman, MS, RD, LDN, is a clinical dietitian based in Chicago.
Learning Objectives
After completing this continuing education course, nutrition professionals should be better able to:
1. Discuss the dietitian’s role in the screening, assessment, and treatment of dysphagia.
2. Compare the National Dysphagia Diet to the International Dysphagia Diet Standardization Initiative (IDDSI).
3. List the eight levels that compose the IDDSI framework.
Examination
1. Dysphagia affects approximately what percentage of the world’s population?
a. 3%
b. 5%
c. 8%
d 12%
2. Which of the following conditions is the leading cause of dysphagia?
a. Gastroesophageal reflux disease
b. Aspiration pneumonia
c. Esophageal cancer
d. Stroke
3. The World Gastroenterology Organisation recommends urgent dysphagia screening in which of the following populations?
a. Patients with chronic gastroesophageal reflux disease
b. Patients with persistent weight loss and recurrent chest infections
c. Infants and adults over the age of 65
d. Older adults in home care programs, nursing homes, and hospitals
4. International Dysphagia Diet Standardisation Initiative (IDDSI) was created in 2013 to address which of the following?
a. Poor adherence to thickened liquids
b. Increasing rates of dehydration and malnutrition among older adults
c. The need for a global standard to define texture-modified foods and thickened liquids
d. Lack of communication when transferring patients from one care setting to another
5. What is the term for difficulty swallowing due to age-related loss of skeletal muscle mass?
a. Presbyphagia
b. Sarcopenic dysphagia
c. Odynophagia
d. Sarcopenia
6. Nearly what percentage of individuals with dysphagia are at risk of malnutrition?
a. 20%
b. 25%
c. 30%
d. 40%
7. What is the primary objective of diet modification?
a. To ensure safety while eating and drinking
b. To improve quality of life for those with dysphagia
c. To ensure foods and drinks are at the correct consistency
d. To prevent malnutrition and dehydration
8. Which of the following contributes to reduced fluid intake in patients on thickened liquids?
a. Poor taste, lack of flavor, and reduced quality of life
b. Unappealing aesthetics and foul odor of thickeners
c. Lack of access to commercial thickeners
d. Inadequate dysphagia care training in clinical and community settings
9. The National Dysphagia Diet classifies thickened liquids from least to most modified as nectarlike, honeylike, and puddinglike, which IDDSI has replaced with ___, ___, and ____.
a. Stage 1, stage 2, stage 3
b. Mildly thick, moderately thick, other thick
c. Mildly thick, moderately thick, extremely thick
d. Syrup, custard, pudding
10. IDDSI testing methods were designed to be easy and accessible, requiring which of the following tools?
a. Fork, syringe, scale
b. Viscometer, moisture analyzer, penetrometer
c. Spoon, fork, scale
d. Fork, spoon, syringe
References
1. Cichero JA, Lam P, Steele CM, et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI framework. Dysphagia. 2017;32(2):293-314.
2. World Gastroenterology Organisation Global Guidelines. Dysphagia: Global Guidelines and Cascades. https://www.worldgastroenterology.org/UserFiles/file/guidelines/dysphagia-english-2014.pdf. Published September 2014. Accessed December 5, 2022.
3. Sura L, Madhavan A, Carnaby G, Crary MA. Dysphagia in the elderly: management and nutritional considerations. Clin Interv Aging. 2012;7:287-298.
4. Wu XS, Miles A, Braakhuis AJ. Texture-modified diets, nutritional status and mealtime satisfaction: a systematic review. Healthcare (Basel). 2021;9(6):624.
5. Ueshima J, Momosaki R, Shimizu A, et al. Nutritional assessment in adult patients with dysphagia: a scoping review. Nutrients. 2021;13(3):778.
6. Namasivayam-MacDonald AM, Morrison JM, Steele CM, Keller H. How swallow pressures and dysphagia affect malnutrition and mealtime outcomes in long-term care. Dysphagia. 2017;32(6):785-796.
7. Rommel N, Hamdy S. Oropharyngeal dysphagia: manifestations and diagnosis. Nat Rev Gastroenterol Hepatol. 2016;13(1):49-59.
8. Heiss CJ, Goldberg L, Dzarnoski M. Registered dietitians and speech-language pathologists: an important partnership in dysphagia management. J Am Diet Assoc. 2010;110(9):1290, 1292-3.
9. International Dysphagia Diet Standardization Initiative. Complete IDDSI Framework detailed definitions. https://iddsi.org/IDDSI/media/images/Complete_IDDSI_Framework_Final_31July2019.pdf. Published July 2019. Accessed December 12, 2022.
10. Full Nutrition Care Manual (NCM) transition to IDDSI Framework by October 2021. International Dysphagia Diet Standardization Initiative website. https://iddsi.org/News/Special-Features/Full-Nutrition-Care-Management-(NCM)%C2%AE-Transition-t. Published January 19, 2021. Accessed December 1, 2022.
11. Wu XS, Miles A, Braakhuis A. The effectiveness of International Dysphagia Diet Standardization Initiative — tailored interventions on staff knowledge and texture-modified diet compliance in aged care facilities: a pre-post study. Curr Dev Nutr. 2022;6(4):nzac032.
12. Malone JC, R AN. Anatomy, Head and Neck, Swallowing. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing; 2023.
13. Pediatric feeding and swallowing. American Speech-Language-Hearing Association website. https://www.asha.org/practice-portal/clinical-topics/pediatric-feeding-and-swallowing/#collapse_3. Accessed December 5, 2022.
14. Fass R. Approach to the evaluation of dysphagia in adults. UpToDate website. https://www.uptodate.com/contents/approach-to-the-evaluation-of-dysphagia-in-adults. Updated October 4, 2023. Accessed December 9, 2022.
15. Adult dysphagia. American Speech-Language-Hearing Association website. https://www.asha.org/practice-portal/clinical-topics/adult-dysphagia/#collapse_2. Accessed December 5, 2022.
16. Swallowing screening. American Speech-Language-Hearing Association website. https://www.asha.org/practice-portal/clinical-topics/adult-dysphagia/swallowing-screening/. Accessed December 5, 2022.
17. Nutrition Care Manual. Academy of Nutrition and Dietetics website. https://www.nutritioncaremanual.org/. Accessed December 10, 2022.
18. Macht M, King CJ, Wimbish T, et al. Post-extubation dysphagia is associated with longer hospitalization in survivors of critical illness with neurologic impairment. Crit Care. 2013;17(3):R119.
19. Belafsky PC, Mouadeb DA, Rees CJ, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117(12):919-924.
20. Zhang PP, Yuan Y, Lu DZ, et al. Diagnostic accuracy of the Eating Assessment Tool-10 (EAT-10) in screening dysphagia: a systematic review and meta-analysis. Dysphagia. 2023;38(1):145-158.
21. O’Keeffe ST. Use of modified diets to prevent aspiration in oropharyngeal dysphagia: is current practice justified? BMC Geriatr. 2018;18(1):167.
22. Fazakerly A, Nativ N. The geriatric swallow: through thick and thin. Perspect ASHA SIGs. 2020;5(4):1039-1044.
23. Brown JE. Nutrition and the older adult. Nutrition Through the Life Cycle. 5th ed. Boston, MA: Cengage Learning; 2014:455-457.
24. McGinnis CM, Homan K, Solomon M, et al. Dysphagia: interprofessional management, impact, and patient‐centered care. Nutr Clin Pract. 2019;34(1):80-95.
25. Cichero JA, Steele C, Duivestein J, et al. The need for international terminology and definitions for texture-modified foods and thickened liquids used in dysphagia management: foundations of a global initiative. Curr Phys Med Rehabil Rep. 2013;1(4):280-291.
26. Wu XS, Miles A, Braakhuis A. Nutritional intake and meal composition of patients consuming texture modified diets and thickened fluids: a systematic review and meta-analysis. Healthcare (Basel). 2020;8(4):579.
27. Cichero JAY. Thickening agents used for dysphagia management: effect on bioavailability of water, medication and feelings of satiety. Nutr J. 2013;12:54.
28. Parsons EL, Stratton RJ, Cawood AL, Smith TR, Elia M. Oral nutritional supplements in a randomised trial are more effective than dietary advice at improving quality of life in malnourished care home residents. Clin Nutr. 2017;36(1):134-142.
29. Stange I, Bartram M, Liao Y, et al. Effects of a low-volume, nutrient-and energy-dense oral nutritional supplement on nutritional and functional status: a randomized, controlled trial in nursing home residents. J Am Med Dir Assoc. 2013;14(8):628-e1.
30. Wu XS, Yousif L, Miles A, Braakhuis A. A comparison of dietary intake and nutritional status between aged care residents consuming texture-modified diets with and without oral nutritional supplements. Nutrients. 2022;14(3):669.
31. Huppertz VA, Van Wijk N, Baijens LW, et al. Design of the DYNAMO study: a multi-center randomized controlled trial to investigate the effect of pre-thickened oral nutritional supplements in nursing home residents with dysphagia and malnutrition (risk). BMC Geriatr. 2020;20(1):537.
32. Dennehy T, Veldkamp F, Lansink M, Schulz RJ. Tolerability, compliance, and product evaluation of a pre-thickened Oral nutritional supplement for disease related malnutrition in patients with dysphagia. J Aging Res Clin Pract. 2020;8:85-90.
33. Felt P. The National Dysphagia Diet Project: the science and practice. Nutr Clin Pract. 1999;14:S60-S65.
34. National Dysphagia Diet Task Force. National Dysphagia Diet: Standardization for Optimal Care. Chicago, IL: American Dietetic Association; 2002.
35. Brewsaugh AM, Brust LJ, Hartman J. Implementing the International Dysphagia Diet Standardization Initiative: opportunities for change. J Acad Nutr Diet. 2022;122(2):270-277.
36. McCullough G, Pelletier C, Steele C. National dysphagia diet: what to swallow? ASHA Lead. 2003;8(20):16-27.
37. Available translations. International Dysphagia Diet Standardisation Initiative website. https://iddsi.org/Translations/Available-Translations. Accessed December 15, 2022.
38. Resources. International Dysphagia Diet Standardisation Initiative website. https://iddsi.org/Resources. Accessed December 27, 2022.
39. IDDSI testing methods. International Dysphagia Diet Standardisation Initiative website. https://iddsi.org/Testing-Methods. Accessed December 12, 2022.
40. International Dysphagia Diet Standardisation Initiative. Common ground between NDD and IDDSI. https://iddsi.org/IDDSI/media/images/Translations/1-Common-Ground-between-NDD-and-IDDSI.pdf. Updated July 2021. Accessed December 15, 2022.
41. International Dysphagia Diet Standardisation Initiative. IDDSI implementation guide: clinicians and health care providers. https://iddsi.org/IDDSI/media/images/ImplementationGuides/Clinicians-and-Health-Care-Providers_IDDSI-Implementation-Guide_Final_3April2018.pdf. Accessed December 12, 2022.
42. Bice EM, Galek KE, Vose AK. A survey of speech pathologist practice patterns for consulting registered dieticians when recommending diet alterations. Speech Lang Hear. 2022;25(1):59-67.



