 November/December 2024 Issue
November/December 2024 Issue
Artificial Intelligence in Dietetics
By Janice MacLeod, MA, RD, CDCES, FADCES
Today’s Dietitian
Vol. 26 No. 9 P. 18
The Value of RDs in an AI-Powered Health Care Revolution
Artificial intelligence (AI) is here and will be a major part of transforming health care, which is predicted to change more in the next decade than it has in the previous century. Why does health care need to change and how will AI help? Health care needs to change because health care is not healthy. This article will discuss how the role of RDs must evolve to demonstrate the profession’s value amid what is being called an AI-powered health care revolution. The RD can lead in harnessing the potential of AI to help make health care healthful.
Six in 10 American adults are living with chronic conditions.1 It’s estimated that 90% of the $4.3 trillion annual cost of health care in the United States is spent on medical care for chronic diseases.2 The increasing prevalence of complex cardiometabolic conditions, combined with a waning number of skilled care providers3 underscores the need for new approaches to chronic care management to expand access to care, lessen the burden of care, improve efficiencies and reduce unsustainable medical costs. The RD plays a critical role in chronic care management since healthful eating as part of a healthy lifestyle is foundational to managing chronic conditions.
It’s reported that primary care providers with a typical panel of 2,500 adult patients would need to work 26.7 hours per day to provide all the recommended preventive, chronic care. While the time demands are still excessive, if a team-based care model (including RDs) is implemented, the hours needed to provide recommended care decrease by over half.4 It’s predicted that generative AI technologies like Chat-GPT will be able to help lessen the workload considerably as AI reliability and capability continue to improve.5 This is an opportunity for RDs well-versed in AI technologies to provide their expertise to boost the value and reach of their services in the primary care setting and beyond.
Artificial Intelligence Defined
What is AI or augmented intelligence as the American Medical Association names it? Table 1 provides definitions, and Table 2 lists ways AI is being used in health care, including in the RD practice, and some potential risks to be aware of.6
Organizations are forming to address the challenges of responsibly bringing AI to health care. One such organization, Coalition of Health AI, includes stakeholders from across the health care and technology landscape to harmonize standards and reporting for health AI and to educate end-users on how to evaluate these technologies. The US National Academy of Medicine is developing a Code of Conduct for AI in health care and biomedical science while the American Board of Artificial Intelligence in Medicine offers training courses and certification on health AI (see sidebar for access to these organizations and other resources). These organizations stress the responsibility all clinicians have to work collaboratively with their respective workplace leadership and colleagues to responsibly leverage AI for the tremendous good it can bring to health care. RDs can join these organizations to provide their expertise and to envision and shape a better health care future.
AI-Powered Technologies Can Help Address Health Care Challenges
The increasing availability of connected health technologies such as episodic and continuous glucose monitors, smart insulin delivery tools (automated insulin delivery and smart insulin pens), blood pressure monitors, fitness wearables, smart scales, heart rate monitors, stethoscopes and other digital health applications enable and empower individuals to measure, track, and self-manage their health directly using the data collected during their daily lives.
AI-powered digital health tools can analyze the various data generated by the person using these connected technologies and provide personalized coaching and feedback as people self-manage their chronic conditions while away from the care team. Clinicians can remotely monitor population-level data to assess the health of the populations they serve. They can efficiently identify who needs human intervention and when, whether a brief coaching nudge or reminder, an adjustment in a therapy prescription, or behavioral or social support (see Figure 1).
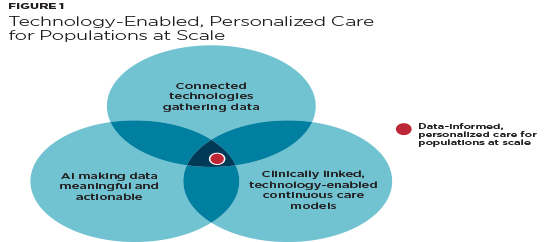
Using text messaging, patient portals, digital social networks, and video telehealth, clinical teams can interact remotely with their clients as needed in a continuous, data-informed feedback loop.7 This better matches the demands of living with a persistent condition like diabetes and other chronic conditions. This enables a pivot away from the inefficient and ineffective episodic, time-bound care model to a continuous, on-demand data-informed care approach that allows each member of the care team to operate at the top of their license, making the most of valuable clinician time. AI-powered health technologies enable the move from mass generalization to mass customization, providing true person-centered care for entire populations at scale.8 Educating on the benefits of connectivity and building digital health literacy skills among those living with chronic conditions as well as addressing the digital divide is critical.9,10

In response to the challenges health care is facing, the Institute for Health Improvement has set forth the quintuple aim: Improving the health of the population (aim 1) at a lower cost (aim 2), while improving both the patient and health care team care experience (aims 3 and 4) and addressing disparities in care (aim 5).11 The fifth aim requires a shift from a downstream and reactive disease management health care approach to an upstream, proactive, and preventive approach. With health inequities estimated to cost the US health care system approximately $83 billion annually, addressing the fifth aim is critical for value and sustainability.12 Finding efficient ways to assess and address social determinants of health (SDOH) through linking to local community resources is essential. AI-enabled geo-location capabilities could identify, for example, local food banks for those struggling with food insecurity. Natural language processing capabilities can be used to efficiently scan free text in medical records where many risk factors for disease severity and progression and SDOH are captured and thus help clinicians and health care systems identify at-risk patients.

Why Do RDs Need to Learn and Join the Conversation?
AI experts see the true potential of AI as giving health care systems the opportunity to rethink and redesign the patient customer care experience from start to finish. As an example, instead of just sending a patient the results of a recent lab draw, alternatively, providing the lab results with an explanation of what the results mean and linking to potential action steps including, if indicated, providing an opportunity to schedule an appointment with an RD to address for example, an abnormal lipid profile. It’s important for RDs to be aware of AI initiatives being explored and implemented to better provide input on how to integrate valuable RD services. Refer to the sidebar for action steps to take to build your AI literacy and join the intelligent health care revolution.
In Conclusion
There’s a golden opportunity for the RD to step up and lead in harnessing the expanding AI-powered digital health capability to build a continuous, data-informed, virtual care model linking people with chronic conditions to expert care on-demand, 24/7, better matching the reality of living with persistent chronic conditions like diabetes. Specialized virtual care and education clinics would need to connect to behavioral health experts and local community resources to help address the SDOH. This requires thinking about and delivering care completely differently, including reimagining the role of the RD.13
Anybody (including a chatbot) can hand out a list of foods to eat and avoid. It takes a skilled RD with expertise in person-centered care to equip and empower a client in progressively building a healthful approach to food that fits their life and promotes wellbeing. As technology advances, RDs have a chance to offload some of the rote, repetitive tasks and finally focus on the person in front of them. A truly transformative revolution such as this brings major opportunities and major challenges. AI is here and it’s up to each one of us to harness its potential to make health care healthful.
— Janice MacLeod, MA, RD, CDCES, FADCES, is a diabetes-cardiometabolic consultant and key opinion leader in digital health and chronic condition management. She is past chair of the Academy of Nutrition & Dietetics Diabetes Practice Group and is currently serving on the Association of Diabetes Care and Education Specialists Board of Directors, 2024–2027. MacLeod has authored multiple publications and developed numerous programs on diabetes nutrition, digital health, and practice transformation. Her passion is developing business-savvy solutions leveraging technology to transform care.
Disclosure: JM is serving as a consultant to Welldoc doing medical writing, evidence strategy, and science calendar management.
Action Steps for Building AI Acumen
Consider following these experts in the application of AI to health care. RDs can add valuable perspectives and discover and promote opportunities for RDs to be at the table by providing thoughtful responses to posts.
• Bertlan Mesko, PhD: MedicalFuturist.com; www.linkedin.com/in/bertalanmesko/
• Eric Topol, MD: www.linkedin.com/in/eric-topol-md-b83a7317/
• Harvey Castro, MD: www.linkedin.com/in/harveycastromd
• Tom Lawry: www.tomlawry.com; www.linkedin.com/in/tomlawry/
• Jan Berger: www.linkedin.com/newsletters/7016868239498444800/
Add to your reading list:
• Lawry T. Hacking Health Care: How AI and the Intelligence Revolution Will Reboot an Ailing System. New York: Routledge; 2023.
• The American Medical Association’s Augmented Intelligence in Medicine, available at www.ama-assn.org/practice-management/digital/augmented-intelligence-medicine.
• The Coalition for Health AI’s Blueprint for Trustworthy AI Implementation Guidance and Assurance for Health Care, available at www.coalitionforhealthai.org/papers/blueprint-for-trustworthy-ai_V1.0.pdf.
• The National Academy of Medicine’s Code of Conduct for AI in Health, Health Care, and Biomedical Science, available at https://nam.edu/programs/value-science-driven-health-care/health-care-artificial-intelligence-code-of-conduct.
Consider enrolling in AI training and certification offerings at the American Board of Artificial Intelligence in Medicine, available at https://abaim.org.
Consider every repetitive task you do over and over each day as you provide consultations, teach classes, and document your visits. How could AI help?
Use the Chat GPT Prompt guide to learn how to refine your prompts to optimize output: CHAT GPT Cheat Sheet by Harvey Castro, MD, an AI expert and medical doctor, available at https://www.linkedin.com/posts/harveycastromd_healthcare-gpt-cheat-sheets-activity-7093963347984863232-BB6P.
Join the RD Facebook group AI Powered Nutrition, available at www.facebook.com/groups/350955327768168. This is a place where RDs can learn from each other about using AI in the field of nutrition. The goal is to get the RD profession involved in the AI revolution.
Make a list of what you could do to bring value to clients if freed from the rote, repetitive tasks.
Read this related LinkedIn post: www.linkedin.com/pulse/healthy-eating-diabetes-person-list-foods-avoid-janice/.
Lean in. Embrace the change. Be part of the solution.
References
1. Boersma P, Black LI, Ward BW. Prevalence of multiple chronic conditions among us adults, 2018. Prev Chronic Dis. 2020;17:200130.
2. Sharma V, Sharma R. Food is medicine initiative for mitigating food insecurity in the United States. J Prev Med Public Health. 2024;57(2):96-107.
3. Dall T, West T, Chakrabarti R, Ruttinger C, Zarek P, Parker O. The complexities of physician supply and demand: projections from 2016 to 2030. American Association of Medical Colleges: Washington D.C.; 2018.
4. Porter J, Boyd C, Skandari MR, Laiteerapong N. Revisiting the time needed to provide adult primary care. J Gen Intern Med. 2023;38(1):147-155.
5. Robert Pearl, MD. LinkedIn website. https://www.linkedin.com/pulse/chatgpt-reduce-clinician-burnout-doctors-embrace-robert-pearl-m-d--itqqc/. Published December 23, 2023. Accessed August 5, 2023.
6. Detopoulou P, Voulgaridou G, Moschos P, et al. Artificial intelligence, nutrition, and ethical issues: a mini-review. Clin Nutr Open Sci. 2023;50:46-56.
7. Phillip M, Bergenstal RM, Close KL, et al. The digital/virtual diabetes clinic: the future is now—recommendations from an international panel on diabetes digital technologies introduction. Diabetes Technol Ther. 2021;23(2):146-154.
8. Sinsky CA, Bavafa H, Roberts RG, Beasley JW. Standardization vs customization: finding the right balance. Ann Fam Med. 2021;19(2):171-177.
9. Macleod J, Scher L, Greenwood D, et al. Technology disparities and therapeutic inertia a call to action for the diabetes care and education specialist. ADCES in Practice. 2021;9(5):1-8.
10. Benda NC, Veinot TC, Sieck CJ, Ancker JS. Broadband internet access is a social determinant of health! Am J Public Health. 2020;110(8):1123-1125.
11. Nundy S, Cooper LA, Mate KS. The quintuple aim for health care improvement: a new imperative to advance health equity. JAMA. 2022;327(6):521-522.
12. Solomon LS, Kanter MH. Health care steps up to social determinants of health: current context. Perm J. 2018;22:18-139.
13. Chatelan A, Clerc A, Fonta PA. ChatGPT and future artificial intelligence chatbots: what may be the influence on credentialed nutrition and dietetics practitioners. J Acad Nut Dietet. 2023;123(11):1525-1531.
