 December 2018 Issue
December 2018 Issue
Update on Iodine
By KC Wright, MS, RDN
Today's Dietitian
Vol. 20, No. 12, P. 24
Learn what population subgroups are at risk of deficiency and ways patients can increase their intake.
Dietitians know there are many underconsumed nutrients within the American diet. And of those underconsumed, potassium, dietary fiber, and vitamin D are considered nutrients of public health concern, according to the 2015–2020 Dietary Guidelines for Americans.
But there's another nutrient that's just as important to public health that dietitians should be discussing with clients regularly: iodine.
Iodine is an essential trace mineral believed, in recent history, to be relatively ubiquitous in the American diet due to the iodization of salt. However, throughout the lifecycle, and as current diet trends and fads persist, several changes in food intake may increase risk of iodine deficiency in certain population groups. In fact, iodine deficiency has become an underrecognized issue. Therefore, dietitians must evaluate iodine status in nutrition assessments.
Iodine is naturally present in some foods, fortified in others, and available in multivitamin/mineral formulas and as individual dietary supplements. It's a vital constituent of the thyroid hormones thyroxine (T4) and triiodothyronine (T3). Thyroid hormones regulate many key biochemical processes, including protein synthesis and enzyme actions. These hormones are critical determinants of metabolic activity and required for normal skeletal and central nervous system development in both the fetus and infant.1,2
Thyroid function is mainly regulated by thyroid-stimulating hormone (TSH), secreted by the pituitary gland to control thyroid hormone function and release, protecting the body from hypothyroidism and hyperthyroidism.1 TSH secretion triggers the thyroid to take up iodine and stimulates the synthesis and release of T3 and T4. Without adequate iodine, TSH levels remain high, leading to goiter—an enlargement of the thyroid gland, reflecting the body's failed attempt to sequester iodine from circulation. Supplementing an iodine-deficient goiter will lead to a reduction in size of the goiter.3
In other physiological functions, iodine appears to play a role in the immune response and may have a beneficial effect on mammary dysplasia and fibrocystic breast disease.2
Regional Iodine Sources
Iodine is naturally present in both soil and seawater. Food products from animals and aquatic life sustained on either soil or seawater contain iodine. Dairy products, especially milk, and grain products are the major contributors of iodine to the American diet. Some regions of the world have soils lacking iodine, increasing the risk of iodine deficiency among people consuming foods mainly from that area, which continues to be a global health problem.
Before the 1920s and the introduction of iodized salt, iodine deficiency was common in the "goiter belt"—the Great Lakes, Appalachian, and the Pacific Northwest, and throughout most of Canada.4 Programs to iodize salt have been implemented in many countries, significantly reducing the prevalence of iodine deficiency worldwide.2,5
Approximately 70% of households worldwide use iodized salt, ranging from almost 90% of households in North and South America to less than 50% in Europe and the eastern Mediterranean regions.6
In food and iodized salt, iodine is present in several forms, including sodium and potassium salts, inorganic iodine, iodate, and iodide, which is the most common form. Once consumed, iodide is quickly and almost completely absorbed in the stomach and duodenum.
When it enters circulation, the thyroid gland concentrates it for thyroid hormone synthesis, while the remainder is lost in urine.2 An iodine-replete healthy adult's body contains about 15 to 20 mg of iodine, 70% to 80% of which is stored in the thyroid.7
Nutrient Needs and Food Sources
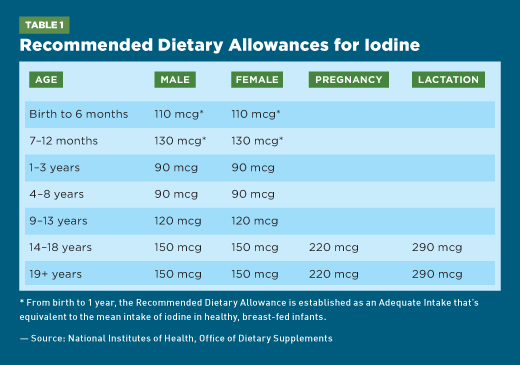
Iodine needs fluctuate throughout the lifecycle, ranging from 90 mcg in toddlers to 290 mcg for breast-feeding women. The current Recommended Dietary Allowances for iodine are shown in Table 1.8
The Total Diet Study, an FDA monitoring program, estimated that the average iodine intake in the US population ranged from 138 to 353 mcg daily across all age and gender groups.9 Total Diet Study data don't include iodine consumed from the discretionary use of iodized salt, and thus may underestimate the true iodine intake of most US residents.10,11
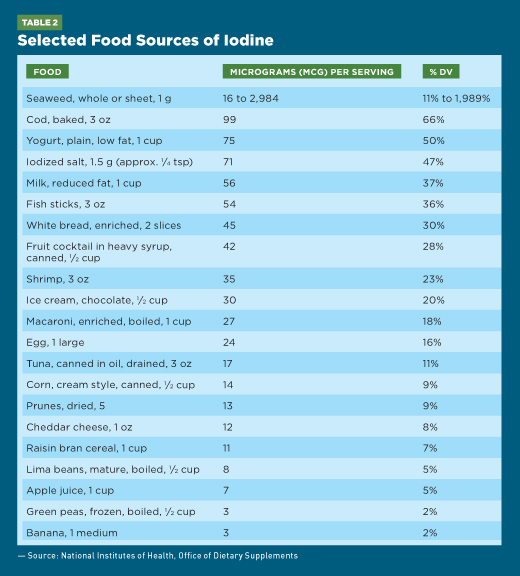
Seaweed, including kelp, nori, kombu, and wakame, is one of the best food sources of iodine, but it's highly variable in content—ranging from approximately 16 to 2,984 mcg per 1-g serving. A 3-oz serving of cod contains almost 100 mcg iodine. Dairy also is a good source of iodine due to the feed supplements and iodophor sanitizing agents used in the dairy industry.10 One cup each of yogurt and milk has 75 and 56 mcg, respectively, whereas two slices of enriched bread have 45 mcg iodine. Breast milk and infant formulas both contain iodine.2,5
The amount of iodine in fruits and vegetables varies depending on the soil's iodine content. Subsequently, this variability affects the iodine content of meat and animal foods because it reflects the iodine content of foods in the animals' diets. Approximately a 1/2 cup of corn contains 14 mcg iodine, while a banana contains just 3 mcg. Table 2 lists selected food sources of iodine.8
A teaspoon of iodized salt in the United States contains about 400 mcg iodine,8 but reducing salt intake isn't likely to affect iodine intake because it provides only a fraction of daily iodine intake for most Americans.12 And, as dietitians are aware, the majority of salt intake in the United States comes from processed foods; food manufacturers almost always use noniodized salt. If iodized salt is used in food processing, it must be listed as iodized salt on the food label ingredient list.9
According to Consumer Lab, many multivitamin/mineral supplements often include iodine—typically 150 mcg from potassium iodide.13 Individual iodine supplements or iodine-containing kelp also are available. Dried kelp powders are about 0.1% to 0.5% iodine, so obtaining 150 mcg iodine would require consuming 30 to 150 mg kelp powder, or less if using extracts (which are more concentrated in iodine).13
Data from the National Health and Nutrition Examination Survey (NHANES) collected between 1999 and 2004 show that 28% to 29% of adults use iodine-containing dietary supplements.14 It's important to consider that iodine supplements have the potential to interact with several types of medications, including methimazole, used to treat hyperthyroidism; angiotensin-converting enzyme, or ACE, inhibitors; and potassium-sparing diuretics.7
When Iodine Deficiency Is a Risk
Measures of urinary levels that reflect dietary intake typically assess iodine status. Under normal conditions, the body tightly controls thyroid hormone concentrations via TSH that's usually secreted when iodine intake falls below 100 mcg daily.5 TSH increases thyroidal iodine uptake from the blood and production of thyroid hormone. However, very low iodine intakes can reduce thyroid hormone production even in the presence of elevated TSH levels. Worldwide, iodine deficiency remains a public health problem in 47 countries—about 2.2 billion people (38% of the world's population) live in areas with iodine deficiency.7,14
If a person's iodine intake falls below approximately 10 to 20 mcg per day, hypothyroidism occurs, frequently accompanied by goiter—usually the earliest clinical sign of iodine deficiency.1,2 In pregnant women, iodine deficiency of this magnitude can cause major neurodevelopmental deficits and growth retardation in the fetus, as well as miscarriage and stillbirth.5 Chronic, severe iodine deficiency in utero causes congenital iodine deficiency syndrome, previously known as cretinism, a condition characterized by multiple physical and neurological abnormalities.5
Iodine deficiency also has multiple adverse effects on growth and development and is the most common cause of preventable mental retardation in the world.15 Iodine deficiency disorders result from inadequate thyroid hormone production secondary to insufficient iodine.5
Women of Childbearing Age and Infants
Although most Western countries are iodine replete, iodine deficiency is recognized as the single most preventable cause of neurological impairment on a global level.6,16 Therefore, health care practitioners should educate pregnant women and women planning pregnancy about the importance of iodine intake and supplementation. Other high-risk groups include children and breast-feeding mothers.
Some countries have taken steps to alleviate the problem. For example, in 2009 in Australia, public health measures aimed at boosting dietary iodine through mandatory iodine fortification of bread were implemented.6,17
As noted in Table 1, iodine requirements increase almost 1.5- to two-fold during pregnancy and lactation, respectively. The American Thyroid Association recommends that women who are planning pregnancy, pregnant, or lactating take supplements containing 150 mcg of iodine daily.3 The addition of iodine in prenatal vitamins isn't mandatory in the United States. Not all prenatal vitamins contain adequate amounts of iodine. In fact, almost one-quarter of 59 different prenatal vitamins marketed between 2016 and 2017 didn't contain iodine.18
Analysis of NHANES datasets from 2001 to 2008 show that a substantial portion of pregnant women in the United States are iodine insufficient.19,20 Previous research has confirmed that there's poor understanding of the consequences of iodine deficiency and that many women don't recognize its importance during pregnancy.21 Current research shows that despite public health strategies, a significant proportion of women of childbearing age remain iodine deficient.16 Pregnant and lactating women who don't consume dairy products may be particularly at risk of iodine deficiency.
Less severe iodine deficiency can cause neurodevelopmental deficits in infants and children such as somewhat lower-than-average intelligence.1,14 Aside from goiter, mild to moderate maternal iodine deficiency also has been associated with an increased risk of ADHD in children and can cause impaired mental function.22 Chronic iodine deficiency also may be associated with an increased risk of the follicular form of thyroid cancer.23
The Influence of Current Diet Trends
The 2015–2020 Dietary Guidelines for Americans recommend vegetarian diets as a healthful dietary pattern.24 In fact, 40% of Americans are actively seeking more plant-based foods to include in their diets.25 Because plant-based diets have the potential to be low in iodine, people who don't consume key vegetarian sources, such as iodized salt or sea vegetables, may be at risk of iodine deficiency.26 Vegans especially should consider supplementation if they don't use iodized table salt or have another dietary iodine source.
RDs continually encourage their clients and the public to consume plenty of nutrient-dense cruciferous vegetables rich in anti-inflammatory compounds. It's worth mentioning that cruciferous vegetables, including broccoli, cauliflower, cabbage, kale, arugula, Brussels sprouts, watercress, and radishes, are high in goitrogens that may interfere with the uptake of iodine in the thyroid and thus perpetuate an iodine deficiency.2 But for most people in the US population who have adequate iodine intakes and eat a varied diet, consumption of foods containing goitrogens need not be a concern.
Women who restrict dietary salt intake also have lower urinary iodine concentrations and may be more at risk of iodine deficiency than women who don't restrict salt intake.22 In many homes and kitchens, a large variety of sea salts, which offer more flavor and health benefits, have displaced standard iodized table salt. The potential health benefits of sea salts include higher concentrations of essential minerals such as calcium, iron, potassium, and magnesium. Yet, they don't have any added iodine. This represents just another small factor if a person is suspected of being iodine deficient.
Another concern is that consumer demand for plant-based milk alternatives has shown phenomenal growth while sales of dairy milk have plummeted.27,28 Most plant milks aren't fortified with iodine; therefore, people who substitute these for dairy foods—naturally rich sources of iodine—may be at increased risk of deficiency.
A recent analysis of the nutrient content of many plant-based milk alternatives on the market in the United Kingdom showed that although many products are fortified with calcium, just three out of 47 nondairy plant beverages were fortified with iodine.29 These data confirm similar outcomes of previous research here in the United States that measured iodine content in a variety of milk alternatives, where far less iodine was found than in dairy products.30 And, as both seafood and dairy are significant sources of dietary iodine, vegans may be at an even greater risk of deficiency.
It's been estimated that between 1 million and 3 million Americans follow some type of Paleolithic (paleo) diet with a protocol that shuns both dairy products and table salt.31 A two-year prospective randomized trial found that a paleo diet results in a higher risk of developing an iodine deficiency when compared with a more varied diet, suggesting that supplementation should be considered when choosing a paleo diet.32
Overconsumption of Iodine: Implications for Health
Ironically, excessive iodine intake can have some of the same symptoms as iodine deficiency—such as goiter, elevated TSH levels, and hypothyroidism—because too much iodine in susceptible individuals inhibits thyroid hormone synthesis and thereby increases TSH stimulation that can produce goiter.4,33
Iodine-induced hyperthyroidism also can result from high iodine intakes, usually when iodine is given to treat deficiency. However, most people are unlikely to exceed the daily tolerable upper intake level for iodine from foods and supplements, which is 900 mcg for those aged 14 to 18 and 1,100 mcg for adults.
Overall, the general US population appears to consume adequate iodine. Though blanket iodine supplementation is unwarranted, continued national iodine monitoring is necessary with emphasis on population subgroups most susceptible to risk of iodine deficiency, specifically women of childbearing age and those following restricted diets. Here, RDs have an opportunity to educate their clients about the need for sufficient iodine intake, with consideration of the 2015–2020 Dietary Guidelines for Americans' affirmation that "nutritional needs should be met primarily from foods."24
— KC Wright, MS, RDN, writes articles based on her research and clinical experiences. She advocates for good food and sustainable food systems at www.wildberrycommunications.com.
References
1. National Research Council of the National Academies. Health implications of perchlorate ingestion. https://www.nap.edu/read/11202/chapter/1. Published 2005.
2. Institute of Medicine, Food and Nutrition Board. Dietary Reference Intakes for vitamin A, vitamin K, arsenic, boron, chromium, copper, iodine, iron, manganese, molybdenum, nickel, silicon, vanadium, and zinc. https://www.nap.edu/read/10026/chapter/1. Published 2001.
3. Goiter. American Thyroid Association website. https://www.thyroid.org/goiter/. Accessed October 26, 2018.
4. UNICEF. The state of the world's children 2007: table 2: nutrition. https://www.unicef.org/publications/files/The_State_of_the_Worlds__Children__2007_e.pdf#
page=116. Published 2006.
5. Zimmermann MB. Iodine deficiency. Endocr Rev. 2009;30(4):376-408.
6. World Health Organization; United Nations International Children's Emergency Fund; International Council for Control of Iodine Deficiency Disorders. Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers, third edition. http://apps.who.int/iris/bitstream/handle/10665/43781/9789241595827_eng.pdf;jsessionid=
8A8D521AC75A591869E20EB6706141D7?sequence=1. Published 2007.
7. Zimmermann MB, Jooste PL, Pandav CS. Iodine-deficiency disorders. Lancet. 2008;372(9645):1251-1262.
8. Iodine: fact sheet for health professionals. National Institutes of Health, Office of Dietary Supplements website. https://ods.od.nih.gov/factsheets/Iodine-HealthProfessional/. Updated September 26, 2018. Accessed September 28, 2018.
9. Murray CW, Egan SK, Kim H, Beru N, Bolger PM. US Food and Drug Administration's Total Diet Study: dietary intake of perchlorate and iodine. J Expo Sci Environ Epidemiol. 2008;18(6):571-580.
10. Pennington JA, Young BE. Iron, zinc, copper, manganese, selenium, and iodine in foods from the United States Total Diet Study. J Food Compost Anal. 1990;3(2):166-184.
11. Pennington JA, Young BE, Wilson DB. Nutritional elements in U.S. diets: results from the Total Diet Study, 1982 to 1986. J Am Diet Assoc. 1989;89(5):659-664.
12. Cut salt — it won't affect your iodine intake. Harvard Health Publishing website. https://www.health.harvard.edu/heart-health/cut-salt-it-wont-affect-your-iodine-intake. Published June 2011. Accessed September 10, 2018.
13. Kelp supplements review. ConsumerLab.com website. https://www.consumerlab.com/reviews/Kelp_Supplements_Review/Kelp/. Updated January 27, 2018. Accessed September 10, 2018.
14. National Health and Nutrition Examination Survey. Centers for Disease Control and Prevention, National Center for Health Statistics website. https://www.cdc.gov/nchs/nhanes/index.htm. Updated October 30, 2018.
15. Santiago-Fernandez P, Torres-Barahona R, Muela-Martínez JA, et al. Intelligence quotient and iodine intake: a cross-sectional study in children. J Clin Endocrinol Metab. 2004;89(8):3851-3857.
16. Andersson M, de Benoist B, Rogers L. Epidemiology of iodine deficiency: salt iodisation and iodine status. Best Pract Res Clin Endocrinol Metab. 2010;24(1):1-11.
17. Burns K, Yap C, Mina A, Gunton JE. Iodine deficiency in women of childbearing age: not bread alone? Asia Pac J Clin Nutr. 2018;27(4):853-859.
18. Patel A, Lee SY, Stagnaro-Green A, MacKay D, Wong AW, Pearce EN. Iodine content of the best-selling United States adult and prenatal multivitamin preparations [published online October 30, 2018]. Thyroid. doi: 10.1089/thy.2018.0386.
19. Caldwell KL, Miller GA, Wang RY, Jain RB, Jones RL. Iodine status of the U.S. population, National Health and Nutrition Examination Survey 2003–2004. Thyroid. 2008;18(11):1207-1214.
20. Caldwell KL, Makhmudov A, Ely E, Jones RL, Wang RY. Iodine status of the U.S. population, National Health and Nutrition Examination Survey, 2005–2006 and 2007–2008. Thyroid. 2011;21(4):419-427.
21. Charlton KE, Yeatman HR, Houweling F. Poor iodine status and knowledge related to iodine on the eve of mandatory iodine fortification in Australia. Asia Pac J Clin Nutr. 2010;19(2):250-255.
22. Vermiglio F, Lo Presti VP, Moleti M, et al. Attention deficit and hyperactivity disorders in the offspring of mothers exposed to mild-moderate iodine deficiency: a possible novel iodine deficiency disorder in developed countries. J Clin Endocrinol Metab. 2004;89(12):6054-6060.
23. Dal Maso L, Bosetti C, La Vecchia C, Franceschi S. Risk factors for thyroid cancer: an epidemiological review focused on nutritional factors. Cancer Causes Control. 2009;20(1):75-86.
24. US Department of Health & Human Services. Dietary Guidelines for Americans 2015-2020: Eighth Edition. https://health.gov/dietaryguidelines/2015/guidelines/. Published January 7, 2016. Accessed September 14, 2018.
25. Plant-based food options are sprouting growth for retailers. Nielsen website. http://www.nielsen.com/us/en/insights/news/2018/plant-based-food-options-are-sprouting-growth-for-retailers.html. Published June 13, 2018. Accessed September 20, 2018.
26. Melina V, Craig W, Levin S. Position of the Academy of Nutrition and Dietetics: vegetarian diets. J Acad Nutr Diet. 2016;116(12):1970-1980.
27. US non-dairy milk market report. Mintel website. https://store.mintel.com/us-non-dairy-milk-market-report. Published September 2017. Accessed September 27, 2018.
28. US sales of dairy milk turn sour as non-dairy milk sales grow 9% in 2015. Mintel website. http://www.mintel.com/press-centre/food-and- drink/us-sales-of-dairy-milk-turn-sour-as-non-dairy-milk-sales-grow-9-in-2015. Published April 20, 2016. Accessed September 27, 2018.
29. Bath SC, Hill S, Infante HG, Elghul S, Nezianya CJ, Rayman MP. Iodine concentration of milk-alternative drinks available in the UK in comparision with cows' milk. Br J Nutr. 2017;118(7):525-532.
30. Ma W, He X, Braverman L. Iodine content in milk alternatives. Thyroid. 2016;26(9):1308-1310.
31. Barclay E. Was 2013 really the year of the paleo diet? National Public Radio website. https://www.npr.org/sections/thesalt/2013/12/27/257669972/was-2013-really-the-year-of-the-paleo-diet. Published December 30, 2013. Accessed September 10, 2018.
32. Manousou S, Stål M, Larsson C. A Paleolithic-type diet results in iodine deficiency: a 2-year randomized trial in postmenopausal obese women. Eur J Clin Nutr. 2018;72(1):124-129.
33. Pennington JA. A review of iodine toxicity reports. J Am Diet Assoc. 1990;90(11):1571-1581.
