June/July 2021 Issue
June/July 2021 Issue
2020–2025 Dietary Guidelines for Americans: What’s New to Share With Clients
By Toby Amidor, MS, RD, CDN, FAND
Today’s Dietitian
Vol. 23, No. 6, P. 12
On December 29, 2020, the 2020–2025 Dietary Guidelines for Americans (DGAs) were released. This version was highly anticipated due to the first-time inclusion of recommendations for infants aged 0 to 24 months and pregnant and lactating women. In addition, the DGAs are organized for the first time by life stage and discuss eating healthfully throughout the life cycle.
The theme of the 2020–2025 DGAs is to “Make Every Bite Count” at every life stage. The manner in which the DGAs are organized is different from how they were structured in the past. The first chapter discusses nutrition recommendations for every life stage, and subsequent chapters are divided by life stage (0 to 24 months, 2 to 18 years, adults, pregnant and lactating women, and older adults). This new format makes it easy for health professionals to navigate the several-hundred–page document.
Below are recommendations that haven’t been seen in previous editions, along with pertinent information from the DGAs.
Nutrition and Health Across the Lifespan
In this first chapter of the DGAs, the following four recommendations are made for every life stage.
1. Follow a Healthy Dietary Pattern at Every Life Stage
Starting at 0 to 6 months, it’s recommended that infants are exclusively breast-fed through at least 1 year of age, and longer if desired. If human milk is unavailable, iron-fortified formula is recommended. At approximately 6 months of age, infants should be introduced to nutrient-dense complementary foods from all food groups. At 12 months through adulthood, a healthful dietary pattern should be followed across the lifespan to meet nutrient needs, help achieve a healthy body weight, and reduce the risk of chronic disease. The healthful dietary patterns suggested in the 2015–2020 DGAs, including the Healthy US-Style, Vegetarian, and Mediterranean-Style, are recommended.
2. Customize and Enjoy Nutrient-Dense Food and Beverage Choices to Reflect Personal Preferences, Cultural Traditions, and Budgetary Considerations
The new DGAs aren’t intended as a prescription but rather provide a framework intended to be tailored to individual needs and preferences, as well as inclusive of the diverse cultures in the United States. A healthful dietary pattern can benefit all individuals, regardless of age, race, ethnicity, or health status. Many examples of culturally diverse foods also are provided, including vegetables such as collards, poke greens, bayo beans, breadfruit, cassava, yuca, and chayote, and fruits such as huckleberries, sapote, guava, and jackfruit.
In addition, the DGAs encourage practitioners to consider their clients’ budgetary constraints and use strategies to help them consume a healthful dietary pattern. Some strategies recommended include considering seasonal and regional foods available and incorporating a variety of fresh, frozen, dried, and canned options.
3. Focus on Meeting Food Group Needs With Nutrient-Dense Foods and Beverages, and Stay Within Calorie Limits
In this edition of the DGAs, food groups and food group subcategories often are referred to throughout the various life stages. One is Total Vegetables, with the subcategories of Dark Green Vegetables; Red & Orange Vegetables; Beans, Peas, and Lentils; Starchy Vegetables; and Other Vegetables. Other groups include Fruits, Dairy, Total Grains (with subcategories of Whole Grains and Refined Grains), and Total Protein Foods, with subcategories of Meat, Poultry, Eggs, Seafood, and Nuts, Seeds, and Soy Products.
A few new items within the food groups include the name change from Legumes to Beans, Peas, and Lentils to more accurately reflect the category of foods included. Beans, peas, and lentils, known as pulses, include dried edible seeds of legumes. In addition, the description under the dairy group explains that only cow’s milk and dairy foods (eg, cheese) and soymilk and yogurt are included in the group. It addresses the question about plant-based beverages and states that other products sold as “milks” made from plants (ie, almond, hemp, coconut, rice, oat) may contain calcium and be consumed as a source of calcium but aren’t included as part of the dairy group because their overall nutritional content isn’t similar to dairy milk and fortified soy beverages.
When it comes to beverages, the DGAs emphasize that the calories and nutrients in beverages are an important consideration in a healthful dietary pattern. Calorie-free beverages (eg, water) are the best choice. In addition, beverages that contribute beneficial nutrients, such as fat-free or low-fat milk and 100% fruit and vegetable juices, are best.
The nutrients of public health concern for every life stage are the same as the previous edition and include fiber, calcium, vitamin D, and potassium.
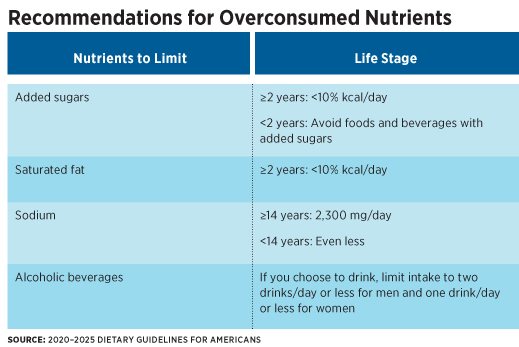
4. Limit Foods and Beverages Higher in Added Sugars, Saturated Fat, and Sodium, as Well as Alcoholic Beverages
For the first time, the DGAs provided recommendations on the percentage of calories that should come from nutrient-dense choices vs other sources. Approximately 85% of calories per day should be allotted to meet food group recommendations healthfully while approximately 15% of calories per day should come from calories available from other, less healthful foods, including those high in added sugars and saturated fat, as well as alcoholic beverages. For most Americans, this is about 250 to 350 kcal per day.
Specific Recommendations for Children and Pregnant Women
Infants and Toddlers (0 through 23 months)
There are several recommendations specific to infants and toddlers aged 0 to 23 months. Supplementation of 400 IU of vitamin D for breast-fed infants is recommended soon after birth. At about 6 months, infants should be introduced to nutrient-dense complementary foods—including potentially allergenic foods. The DGAs state that adding peanut-containing foods to their diet in the first year reduces infants’ risk of developing an allergy to peanuts. Full-fat cow’s milk as a beverage should be introduced at 12 months or later. If an infant is at high risk of a peanut allergy, then age-appropriate peanut-containing foods should be introduced as early as 4 to 6 months to help reduce the risk of developing a peanut allergy. It’s recommended to check with a health care provider before feeding high-risk infants peanut-containing foods; a blood test or skin prick test may be recommended first.
Infants who are fed human milk should be encouraged to eat foods high in iron and zinc. Added sugars should be avoided and foods and beverages high in sodium should be limited. Once infants are weaned from human milk or infant formula, they should transition to a healthful dietary pattern. Although human milk has sufficient vitamin B12 to meet infant needs, if the mother’s vitamin B12 status is inadequate, or the mother is vegan, both the mother and the infant may need vitamin B12 supplementation. Other nutrients of concern include vitamin D, choline, and potassium for older infants.
Honey and unpasteurized foods and beverages (eg, unpasteurized juices, milk, and cheeses) should be avoided due to potentially pathogenic bacteria. Supplemental water isn’t typically needed up to 6 months of age. Small amounts (4 to 8 fl oz/day) of plain, fluoridated drinking water can be given to infants with the introduction of complementary foods. Plain fluoridated drinking water can slowly be increased over one year to meet hydration and fluoride needs. One hundred percent fruit and vegetable juice should be avoided before 12 months of age and isn’t necessary after 12 months. If juice is offered after 12 months, no more than 4 fl oz per day is recommended.
Pregnancy and Lactation
Special nutrient needs for women who are pregnant or planning to become pregnant include a prenatal vitamin and mineral supplement. However, lactating women’s use of prenatal vitamins and minerals may exceed folic acid and iron requirements. They shouldn’t exceed the Tolerable Upper Intake Level of 1,000 mcg of folic acid per day and 45 mg iron per day. Iron needs increase during pregnancy; however, iron needs decrease and return to prepregnancy levels once menstruation resumes.
Iodine needs increase substantially during pregnancy, as it’s important for neurocognitive development of the fetus. Although iodine intake generally is adequate, if a pregnant or lactating woman doesn’t consume dairy products, eggs, seafood, or iodized salt, she may not be getting enough. If using table salt, iodized salt is recommended. If they don’t use table salt, they shouldn’t be encouraged to start. A supplement also may be needed to achieve adequate intake.
Choline requirements increase during pregnancy and lactation. Adequate intake is needed to replenish maternal stores and support growth and development of the child’s brain and spinal cord. Meeting needs through food intake is preferred, but a supplement may be needed. Caffeine passes from the mother to the infant in small amounts through breastmilk but usually doesn’t affect the infant when the mother consumes less than 300 mg per day (about 2 to 3 cups of coffee).
Lastly, this life stage presents a high risk of foodborne illness. Seafood, meats, poultry, and eggs should be cooked to minimum internal cooking temperatures. Unpasteurized juice and milk, raw sprouts, and some soft cheeses made from unpasteurized milk should be avoided. Deli and luncheon meats and hot dogs should be reheated to 165˚ F to kill Listeria.
Counseling Strategies for Dietitians
The DGAs are designed to help all individuals and their families consume a healthful, nutritionally adequate diet. The translation of the DGAs into actionable consumer messages and resources is crucial to help people and their communities follow healthful dietary patterns. MyPlate is one example of how healthful eating can be translated to consumers, who can use and adapt it in various settings to meet personal preferences, cultural foodways, traditions, and budgetary needs. The MyPlate recommendations include filling one-half of the plate with fruits and vegetables, one-quarter of the plate with starches, and one-quarter of the plate with a protein. Include a portion of low-fat or nonfat dairy milk, soymilk, or yogurt with the meal.
When discussing MyPlate with clients, suggest they focus on whole fruits and vary their vegetables. One-half of daily grains should be whole, and they should consume a variety of proteins. In addition, recommend clients choose foods and beverages with fewer added sugars, saturated fat, and sodium. Action is needed on many fronts to ensure healthful dietary choices are affordable and accessible to everyone. Health professionals, communities, businesses and industries, organizations, governments, and other segments of society have a role to play in helping the public make choices that align with the DGAs and ensure access to healthful and affordable food to achieve better health.
— Toby Amidor, MS, RD, CDN, FAND, is the founder of Toby Amidor Nutrition (tobyamidornutrition.com) and a Wall Street Journal bestselling author. She’s written several cookbooks, including The Best 3-Ingredient Cookbook and The Best Rotisserie Chicken Cookbook. She’s also a nutrition expert for FoodNetwork.com and a contributor to U.S. News Eat + Run and other national outlets.
Resource
1. US Department of Agriculture; US Department of Health and Human Services. 2020–2025 Dietary Guidelines for Americans. https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf. Published December 2020.